The appearance of type 2 diabetes in children and teens puzzled physicians from the start. Fida Bacha recalls working as a pediatric endocrinology fellow in Pittsburgh shortly after 2000 when young, overweight and obese patients began to arrive at the clinic, some describing increased thirst, more frequent trips to the bathroom and other symptoms of what was then called adult-onset diabetes.
“It was a new realization that we are dealing with a disease that used to be only an adult disease that is now becoming a disease of childhood,” says Bacha, who practices at Texas Children’s Hospital in Houston.
More than two decades later, physicians and researchers are still trying to unravel what’s driving the emergence and proliferation of youth-onset disease, particularly among marginalized communities including Hispanics/Latinos. The increasing prevalence of obesity among young people is clearly one contributor, but researchers are also scrutinizing the potential influence of other lifestyle and environmental factors — everything from exposure to chronic stress and air pollution to sugar-rich diets. Along with physiological factors, such as where they carry excess fat, youths from lower socioeconomic levels may be vulnerable due to aspects of daily life beyond their control, such as more limited access to healthy food and opportunities to safely exercise in less-polluted neighborhoods.
As researchers try to sort out the interplay among genetics, metabolic factors and environmental influences in Hispanic and other populations, their goal is to answer this key question: Why do some seemingly at-risk adolescents progress to diabetes while others do not?
Long-term, the challenges and health stakes are significant. When type 2 diabetes first emerged in youths, clinicians initially thought its progression would mirror that in adults and thus could be treated accordingly. That hasn’t panned out, says Barbara Linder, a pediatric endocrinologist and senior advisor for childhood diabetes research at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). For instance, researchers have determined that metformin, a commonly prescribed oral antidiabetic medication in adults, doesn’t work as well in young people.
“We know that the disease is very aggressive in youth and very difficult to treat,” Linder says. “So it’s really imperative that we develop effective approaches to prevention. And to do this we obviously need to be able to effectively identify which youth are at the highest risk.”
Even with treatment, young people develop other medical problems related to diabetes faster than adults, according to a study that followed 500 youths, more than one-third of them Hispanic. Sixty percent developed at least one complication within about 15 years after diagnosis, when just in their 20s.
“It’s really alarming,” says Luisa Rodriguez, a pediatric endocrinologist who studies type 2 diabetes and obesity in children at the University of Texas Health Science Center at San Antonio. For every 10 adolescents with youth-onset diabetes, she points out, “six of them, within a decade span, are going to develop a significant comorbidity that will highly impact their lifespan and quality of life.”
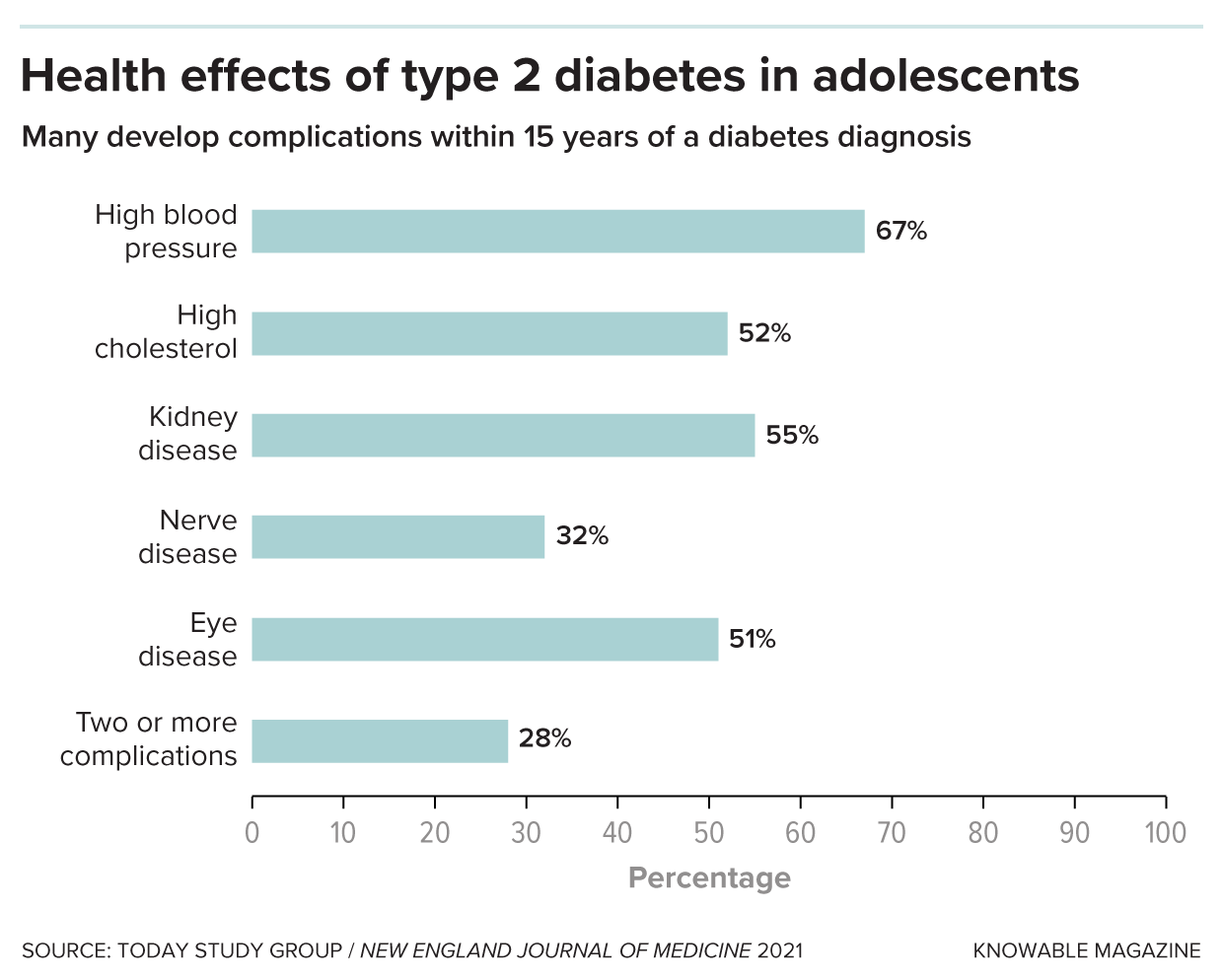
Complications of diabetes appear more quickly in young people than in older adults. Researchers studied 500 overweight adolescents, aged 10 to 17, who had been diagnosed with type 2 diabetes. Within 15 years of their diagnosis, 60 percent of the participants had developed at least one medical complication of diabetes, and 28 percent had developed two or more.
Insulin resistance
In type 2 diabetes, the body struggles to use insulin effectively. This vital hormone, made by beta cells in the pancreas, helps glucose in the bloodstream enter cells in muscle, fat and the liver, where it’s used for energy. But sometimes those cells gradually lose their ability to respond to insulin, forcing the beta cells to pump out more and more of it. If the beta cells can’t keep up, blood glucose levels will begin to rise, leading to a diagnosis of prediabetes and, eventually, diabetes.
In the past, type 2 diabetes typically didn’t arise until well into adulthood. But now, cases in US youths ages 10 to 19 are rising fast. Since 2002-2003, overall diagnoses have doubled from 9 per 100,000 youths to 17.9 per 100,000 in 2017-2018, particularly among Asians, Pacific Islanders, Blacks and Hispanics. If those rising rates persist, the number of type 2 diabetes cases in young people is projected to skyrocket from 28,000 in 2017 to 220,000 by 2060.
Various factors have been linked to insulin resistance in childhood or adolescence, including obesity, inactivity and genetics, according to a review of the causes of type 2 diabetes in youths published in the 2022 Annual Review of Medicine. The disease tends to run in families regardless of race or ethnicity, which suggests that genes matter. Among US Hispanics, adults of Mexican or Puerto Rican heritage are most likely to be diagnosed, followed by Central and South Americans and Cubans.
Obesity is also a contributing factor: Slightly more than one-fourth of Hispanic youths are obese, a higher percentage than for any other major racial or ethnic group. Children also are more likely to develop type 2 diabetes if their mother has the disease or developed gestational diabetes during pregnancy. One theory is that fetal exposure to maternal diabetes while in the womb can spur metabolic changes following birth.
Puberty is also highly influential — most cases are diagnosed after its onset. During puberty, youths temporarily experience insulin resistance, due in large part to an increase in hormones, Linder says. Most youths offset that transient resistance by secreting more insulin, she says. But for reasons that are still unclear, a subpopulation of adolescents does not. “When they’re faced with this stress test of puberty, they can’t increase their insulin secretion enough to compensate,” Linder says. “And that’s probably why they develop type 2 diabetes.”
One analysis, which looked at type 2 diabetes trends from 2002 to 2018, identified the peak age for diagnosis as 16 years in boys and girls. The sole exception involved Black youths, in whom diagnoses peaked at 13 years, and possibly earlier among Black girls, which may be linked to an earlier start of menstruation.
American Diabetes Association guidelines recommend that clinicians screen overweight or obese youths for the disease starting at age 10 or once puberty starts, whichever is earlier, if they have one or more risk factors. These include a family history of the disease, signs of insulin resistance or affiliation with certain racial/ethnic groups, including Hispanic/Latino.
During checkups, clinicians can look for a visible sign of insulin resistance, an associated skin condition called acanthosis nigricans, says Paulina Cruz Bravo, a physician and diabetes researcher at Washington University School of Medicine in St. Louis. The skin changes tend to appear in the neck area or along folds in the skin, including in the armpits and on the elbows and knees, she says. “The top layer of the skin gets thickened. It’s described as a velvety appearance of the skin — it’s darker compared to the skin in other places.”

The thickened, darker, velvety skin shown here, known as acanthosis nigricans, is a potential warning sign of developing type 2 diabetes. The condition is likely to appear on the neck, elbows, knees and other areas where the skin folds. People who notice acanthosis nigricans on themselves or their children should bring it to a doctor’s attention.
CREDIT: S. DULEBOHN / STATPEARLS 2024
Where an adolescent carries any excess pounds also matters, as insulin resistance has been associated with a type of fat called visceral fat, says Alaina Vidmar, a pediatric endocrinologist at Children’s Hospital Los Angeles. Unlike the more common type of fat, called subcutaneous and felt by pinching around the waistline, visceral fat surrounds the liver and other vital organs, increasing the risk for type 2 diabetes, fatty liver disease and other conditions.
“You really need the liver to process glucose to be able to utilize your insulin well,” Vidmar says. “And if it is full of fat, you are unable to do that.” Fatty liver disease, which has been associated both with obesity and type 2 diabetes, is most common in Hispanic adults, followed by white adults and Black adults, according to a meta-analysis looking at 34 studies.
Imaging scans would be the ideal way to identify the extent and location of visceral fat in adolescents, Vidmar says. But given that routine scanning would be costly, clinicians can instead measure an adolescent’s waist circumference, “a great surrogate marker,” she says.
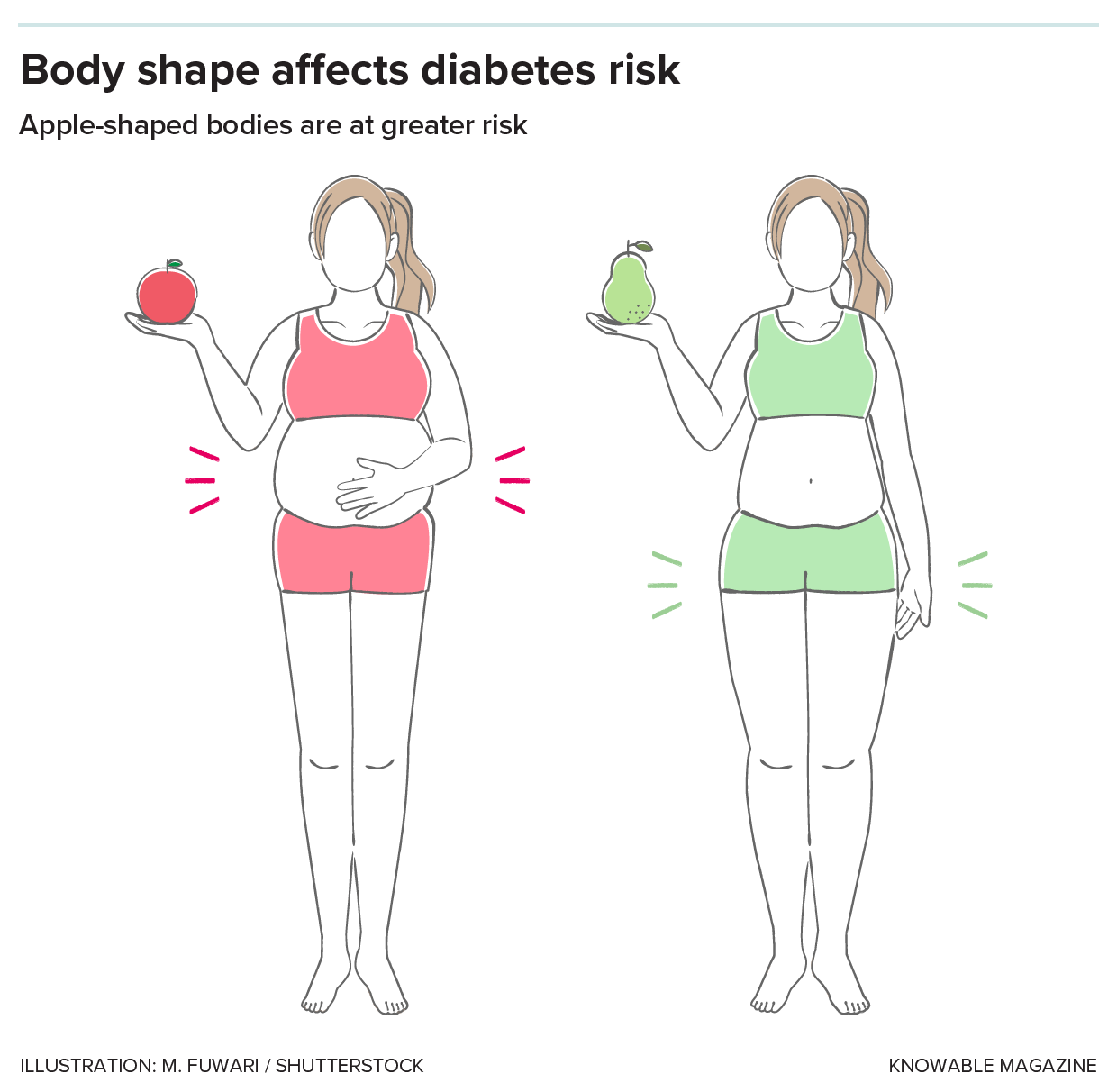
Diabetes risk depends not just on how much fat you carry, but where you carry it. People with an “apple” body shape, with much of their fat in the abdomen, are at higher risk of diabetes than those with a “pear” body shape, who carry their fat under the skin, especially on the hips.
Still, obesity accounts for only a portion of the type 2 risk profile, reflecting the complexities involved in understanding the pathophysiology of youth-onset disease. Roughly one-fourth of youths with type 2 diabetes are not obese, according to a meta-analysis published in 2022 in JAMA Network Open. Asian youths are least likely to be obese; roughly one-third don’t meet the criteria for obesity.
Moreover, while obesity and insulin resistance boost the risk of developing diabetes, those factors alone don’t predict whether an adolescent is eventually diagnosed with the disease, according to the authors of the Annual Review of Medicine overview. Instead, they point to the role of impaired beta cell function.
In one study involving 699 youths with type 2 diabetes, the standard antidiabetic drug metformin controlled blood glucose levels in only about half the participants. (The medication was least effective among Black youths, for reasons that are unclear, according to the researchers.) Another analysis of the same study population identified a 20 percent to 35 percent decline in beta function each year in diabetic youths, compared with prior studies showing about a 7 percent to 11 percent annual decline in diabetic adults.
“What we see in the youth is that beta cell function fails very rapidly,” Linder says, adding that the beta cell decline tends to correlate with the lack of response to metformin.
It’s unknown whether specific racial or ethnic groups are more vulnerable to loss of beta cell function, says Linder, who hopes that a new large-scale NIDDK study launching this summer will identify any such physiological and other differences among populations. The study, called Discovery of Risk Factors for Type 2 Diabetes in Youth Consortium, aims to enroll 3,600 overweight or obese adolescent boys and girls, 36 percent of them Hispanic. Bacha and other investigators on the project plan to follow the youths through puberty, looking at genetic and physiological markers such as insulin resistance and beta cell function. Their goal is to track who develops type 2 diabetes and what factors precipitate the disease.
In addition, researchers will learn about the participants’ mental health, lifestyles and social determinants of health, Linder says. To that end, families will be asked to share details about nutrition, physical activity and sleep, as well as food insecurity, exposure to racism and other stressors.
“Stress induces certain hormones that antagonize insulin, so they create more insulin resistance,” Linder says. “Stress also is associated with chronic inflammation in the body, which affects the ability of the body to respond normally.”
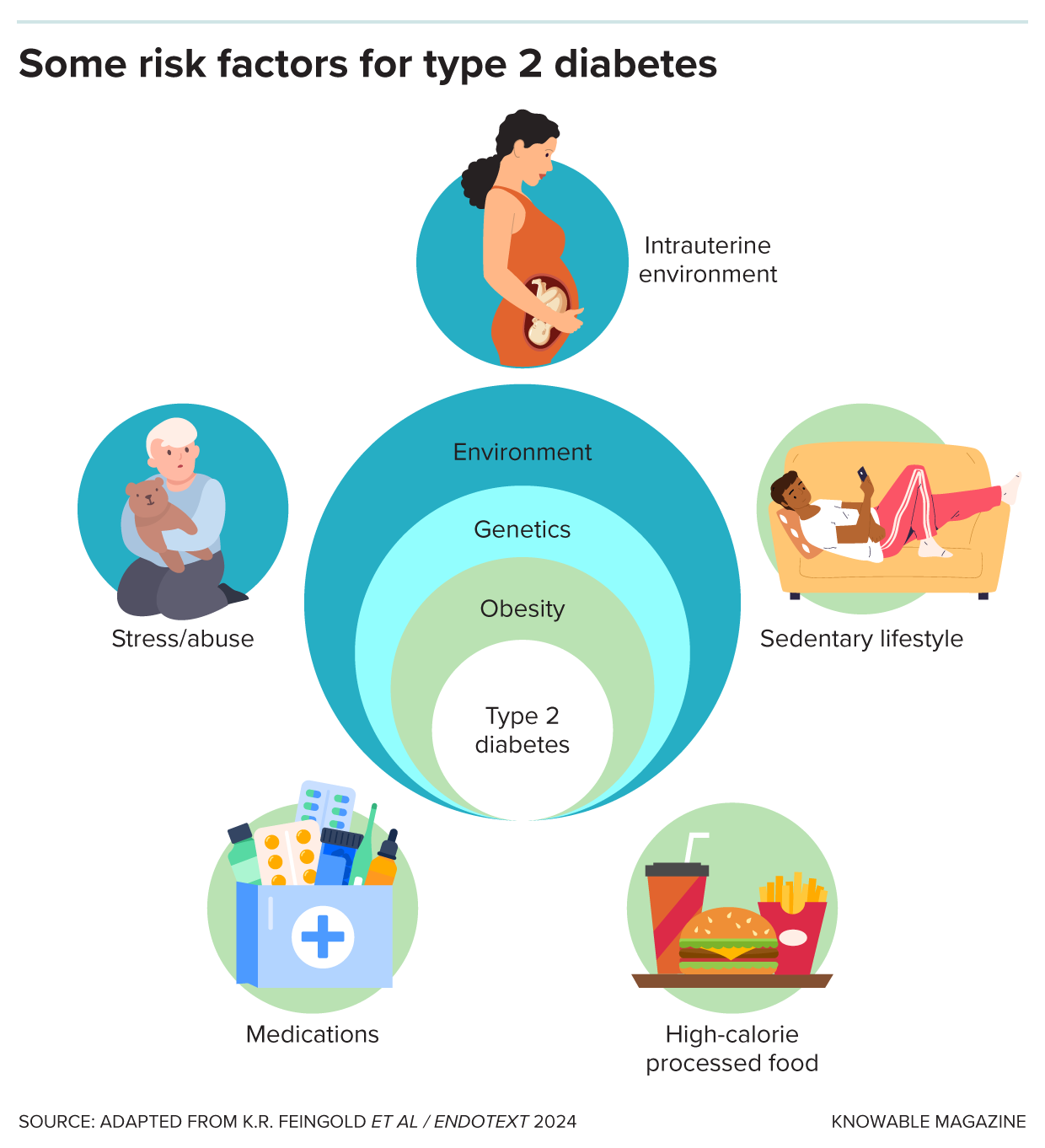
Young people experience many of the risk factors that predispose people to type 2 diabetes, such as prenatal exposures, junk food, sedentary lifestyles and high levels of stress.
Zooming in on risk factors in Hispanic kids
Already, researchers who have studied at-risk Hispanic youths and their families have begun to flesh out environmental and other influences rooted in daily life that can boost the likelihood of obesity or diabetes. Michael Goran, a child obesity researcher at Children’s Hospital Los Angeles, has led a research project called the Study of Latino Adolescents at Risk (SOLAR), which tracked 328 Hispanic/Latino youths considered at highest risk of youth-onset diabetes based on their body mass index and family history of the disease. The participants, recruited in two waves between 2000 and 2015, completed health questionnaires and underwent annual exams, including imaging scans and other measurements.
One analysis found that Hispanic youths who lived in neighborhoods with higher levels of air pollution were more likely to experience a breakdown in beta cell function. “Which we weren’t necessarily expecting — we don’t know the mechanism of that,” says Goran, who coauthored a close look at pediatric insulin resistance in the 2005 Annual Review of Nutrition.
In more recent years, he’s turned his attention to studying nutrition shortly after birth, with a focus on infant formulas that contain corn syrup. Those formulas are more likely to spike blood sugar than are lactose-based formulas, he says. “If you’re spiking blood glucose with corn syrup in babies,” he says, “you can see how that would be problematic for long-term control of blood sugars.”
In one study, Goran and colleagues looked at obesity trends in 15,246 children who received formula through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Babies who consumed any formula with corn syrup were 10 percent more likely to be obese by age 2 than babies who didn’t. Nearly 90 percent of the study’s participants were Hispanic.
In other research, epidemiologist Carmen Isasi of the Albert Einstein College of Medicine in New York helped lead the Study of Latinos (SOL) Youth study, which delved into the extent to which a child’s family circumstances contribute to obesity and metabolic changes that may boost risk of youth-onset diabetes. Isasi and colleagues found chronic stress to be pervasive. Three-quarters of parents and caregivers reported stress and 29 percent detailed three or more stressors related to health, work or relationships. The higher the number of parental stressors, the more likely the child was to be obese.
Isasi also has looked at the relationship between food insecurity and metabolic health. Hispanic youths raised in households with the highest levels of food insecurity had significantly worse metabolic results, including elevated blood glucose and triglycerides, a type of cholesterol. Families dealing with food insecurity, Isasi says, probably have a lower-quality diet and skimp on costlier protein and fresh produce.
Preventing diabetes has proved challenging. A review paper looking at diet-related and other lifestyle initiatives targeting Hispanic youths found few studies to date that have shown improvements in body mass index or blood glucose levels.
Adolescents of lower socioeconomic status may also shoulder responsibilities that can undercut efforts to stay healthy, says Erica Soltero, a behavioral scientist at Houston’s Baylor College of Medicine, who works with Hispanic youths. For instance, older teens may struggle to attend an exercise class if they have an after-school job or must pick up younger siblings or start dinner. Technology, Soltero says, may be a better way to reach busy Hispanic teens; she’s piloting a study that will provide text-based lifestyle guidance to Hispanic teens with obesity.
Approved medication options remain limited for children and teens. If metformin doesn’t work, the alternative is insulin, and parents may resist giving injections because of the difficulties involved, Rodriguez says. She’s involved with an ongoing study in youths with type 2 diabetes to study the effectiveness of oral semaglutide, one of the newer diabetes drugs that also has achieved notable weight loss. Rodriguez estimates the results will be available by 2026.
The new NIDDK study won’t assess medication treatments, as it’s an observational study. But researchers involved are bullish that study-related insights could lead to better prevention and treatment approaches. “If someone is predisposed to beta cell dysfunction, should we be much more aggressive in treating their overweight/obesity,” Bacha says, “so that this beta cell function is preserved for a longer period of time?” Doctors could, for example, decide to start treatment earlier, she says.
Neither are researchers like Soltero deterred by the long-standing difficulties involved with revamping lifestyle habits. Soltero, who has worked with overweight and obese Hispanic adolescents to improve exercise and make dietary changes, describes them as often highly motivated given the damage they’ve seen the disease inflict on their own families.
“A lot of times they’ll have a touch point with a relative who’s on dialysis and maybe had a digit amputated,” Soltero says. Or “they’ll say, ‘I don’t want to prick myself every day like my Uncle So-and-So.’ Or ‘I don’t want to be on medicine for the rest of my life like my grandma.’ ”
This story is part of Knowable Magazine’s Spanish-language series on science that affects or is conducted by Latinos in the United States, supported by HHMI’s Science and Educational Media Group.